People often used to panic when their doctor said they had lung adenocarcinoma in situ (AIS) after a check-up. After all, AIS was once considered a pre-cancer or even a form of cancer. But doctors can now reassure you: there’s no need to fear. That’s because, as of the March 2021 WHO classification of lung tumors, experts no longer classify adenocarcinoma in situ as cancer. They have removed it from the list of malignant tumors.
What is adenocarcinoma in situ (AIS)?
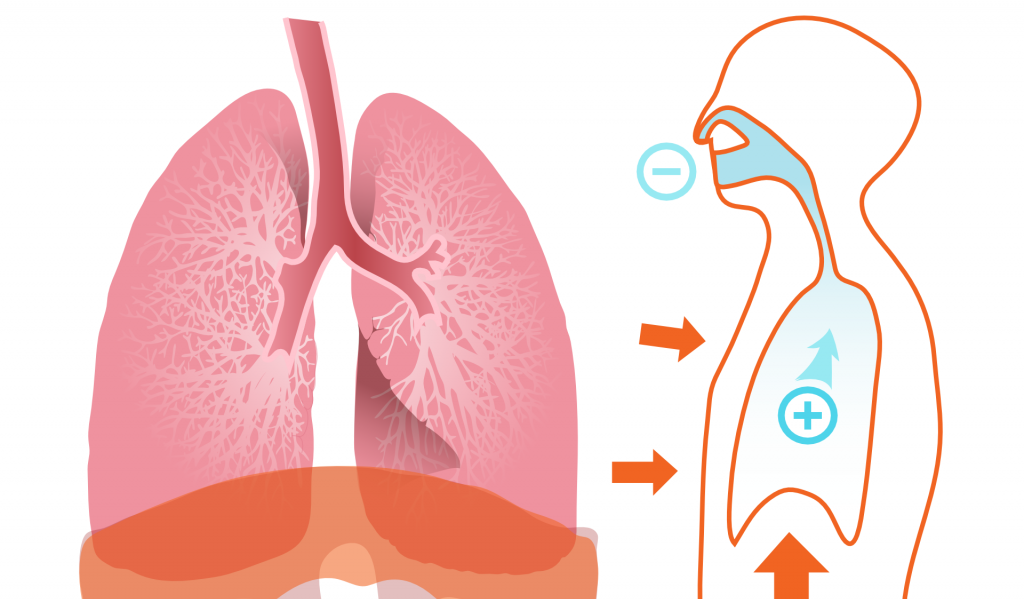
Adenocarcinoma in situ is a cluster of abnormal cells that remain within the epithelium. These cells do not invade nearby normal tissues.
Because of this, doctors no longer consider AIS a true cancer. Instead, they view it as a lesion that might—or might not—develop into cancer later.
On imaging scans, AIS usually appears as a ground glass nodule. Its size and features typically stay the same over time. People with AIS have similar survival quality and life expectancy as those without it.
AIS grows very slowly and can stay within the epithelial layer for many years. In fact, especially in older people, many cases never progress to lung cancer. As a result, doctors often recommend no treatment at all.
Even when treated, AIS has an excellent cure rate and prognosis.
What does it mean that AIS is no longer considered cancer?
Since AIS is no longer classified as cancer, doctors can reduce unnecessary follow-up CT scans. Usually, one scan per year is enough. Patients also avoid many tumor-related tests.
Additionally, people whose ground glass nodules suggest AIS—or those already diagnosed—no longer need to choose surgery.
Which lung nodules are likely to be AIS?
On a CT scan, adenocarcinoma in situ usually shows up as a ground glass nodule (GGN). Most appear as pure ground glass nodules (pGGN); a few are part-solid (PSN).
Key features include:
- Size between 5–30 mm (mostly under 1 cm)
- Uniform density with a CT value under –630 HU
- Possible signs: burrs, vacuoles, or blood vessels passing through—but no curved vessels
- No change in the nodule over long-term follow-up