Doctors often spot lung nodules on chest scans—these are small, well-defined lesions (no bigger than 3 cm across) that sit inside lung tissue filled with air. But not all lung nodules are the same—they split into two main types based on how dense they look: solid nodules and sub-solid nodules.
What’s the difference between solid and sub-solid nodules?
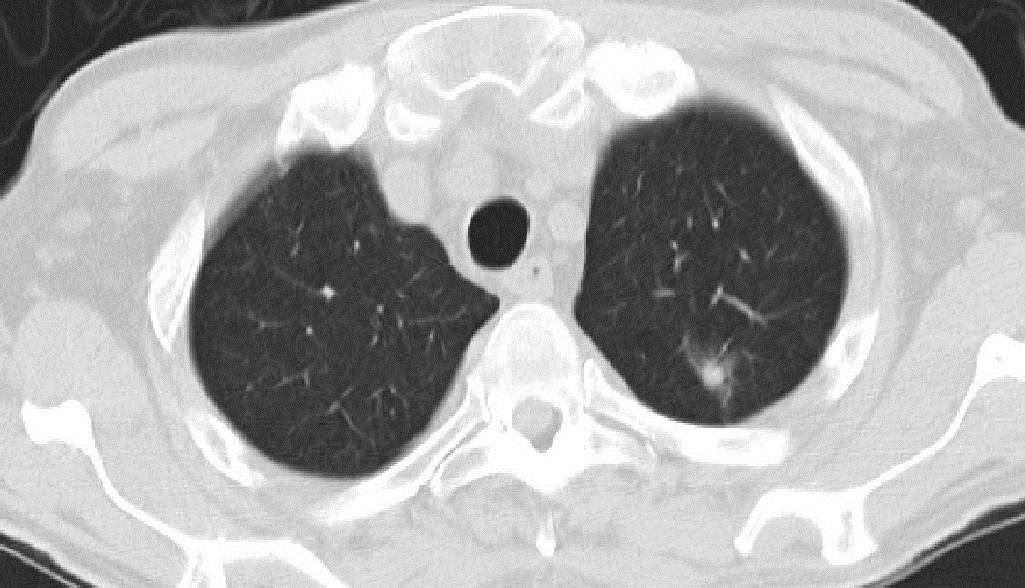
On a CT scan, solid nodules show up as round or oval white spots. They’re dense enough to block the view of the small airways (bronchi) and blood vessels that run through the lung.
Sub-solid nodules, though, are what doctors call ground glass nodules (GGNs)—or sometimes ground glass opacities (GGOs). They break down into two smaller groups:
- Pure ground glass nodules (pGGNs): These have no solid parts at all.
- Mixed ground glass nodules (mGGNs): These have some solid bits mixed in with the hazy part.
What does a GGN look like, and what does it mean?
A GGN shows up on a chest CT as a faint, hazy spot—kind of like looking through frosted glass. It’s less dense than a solid nodule, so you can usually see the blood vessels and bronchi inside it.
Some GGNs will even disappear on their own over time—that usually means they’re from inflammation or other benign (non-harmful) issues. But if a GGN sticks around? It might signal something more serious, like a precancerous lesion, early-stage lung cancer that’s still “in place” (called in-situ lung cancer), or even early invasive lung cancer. That’s why regular follow-up matters.
What causes GGNs?
GGNs can come from a range of conditions, including:
- Scarring in the lungs (interstitial fibrosis)
- Fungal infections in the lungs
- Small, non-cancerous growths (atypical adenomatous hyperplasia)
- Early-stage lung cancers (like in-situ adenocarcinoma, microinvasive adenocarcinoma, or invasive adenocarcinoma)
- Cancer that spread to the lungs from other parts of the body (metastatic lung cancer)
How do doctors tell if a GGN is benign or malignant?
Pulmonologists (lung doctors) look at four key features of the GGN to judge if it’s harmless or risky:
Size
The size of the GGN—especially the solid part—matters a lot. Smaller GGNs are usually benign, while bigger ones are more likely to be malignant. Doctors typically suggest follow-up scans for GGNs bigger than 8 mm to watch for changes in size or density. On the flip side, GGNs smaller than 5 mm have a very low chance of being cancerous.
Margin (Edge of the Nodule)
The edge of the GGN gives clues too. Malignant GGNs often have irregular edges, a “lumpy” shape (called lobulation), or tiny, hair-like spikes (called spiculation). Lobulation, in particular, is more common with cancer and needs attention—but keep in mind: some benign GGNs can also have lobes or spikes, so this isn’t a “sure sign” on its own.
Density
As we talked about earlier, GGNs are less dense than solid nodules. But their density still matters for cancer risk:
- Solid nodules usually have a lower chance of being malignant.
- Pure GGNs have a higher cancer risk than solid nodules.
- Mixed GGNs (with solid parts) have an even higher chance of being malignant.
Growth Rate
Cancerous tumors often grow fast—so if a GGN gets bigger quickly, it’s more likely to be malignant. That’s why follow-up scans (to check if it’s growing) are so important.
What to do if you have a GGN?
First, don’t panic! Most GGNs—especially small ones—aren’t cancerous. But since some GGNs might turn into something serious, you’ll need to see a lung specialist for regular monitoring and follow-up. They’ll track the GGN over time and decide if you need treatment later on.